Which statement is NOT true regarding the ICD-10-CM coding guidelines for burns?
The patient has a ruptured aneurysm in the popliteal artery. The provider makes an incision below the knee and dissects down and around the popliteal artery. After clamping the distal and
proximal ends of the artery, the provider cuts out the defect, sutures the remaining ends of the artery together, and places a patch graft to fill the gap. What is the correct CPT® code for the
aneurysm repair?
A cardiologist performs and interprets a 12-lead ECG in the office.
What CPT® coding is reported?
(Full Case:Preoperative diagnosis:Low back pain; possible spinal stenosis L3–4.Postoperative diagnosis:No evidence of discogenic pathology or spinal stenosis at L3–4; normal discography L3–4.Procedure:Awake discography and injection, L3–4.Anesthesia:IV narcotic with reversal and local; propofol given transiently, then patient alert/responsive for pain response during injection.Technique:Patient to OR; right decubitus; sterile prep/drape; C-arm used to mark entry; local ethyl chloride + 1% Xylocaine; docking needle placed posterolateral at L3–4 under AP/lateral; inner needle advanced to disc nucleus center; contrast injected while monitoring patient response; normal bilocular pattern; 1.5 cc volume; no pain with pressurization.Documentation:No videotape; plain films available; post-discography CT planned/reviewed for other causes.Question:What CPT® and ICD-10-CM coding is reported?)
A patient who was training for a marathon collapsed due to heat exhaustion on a very hot day. The patient is driven by his wife to a non-facility urgent care center for him to be treated. On
examination, the physician diagnoses heat exhaustion and dehydration. The physician began IV therapy of normal saline that consists of pre-packaged fluid and electrolytes. The hydration lasts
for 1 and 30 minutes.
What CPT® coding is reported?
(A 50-year-old patient undergoesflexible bronchoscopy with bronchial biopsies. Five biopsies are taken and sent to the lab. What CPT® coding is reported?)
In medical terminology, suffixes indicate the procedure, condition, disorder, or disease.
Which term contains a suffix?
(A patient has nausea with several episodes of emesis and severe stomach pain due to dehydration. Normal saline is infused in the same bag with2 mg ondansetron. Then15 mg ketorolac tromethamineis given for stomach pain. What J codes are reported for these services?)
(A 62-year-old with insulin-dependent diabetes mellitus has sudden hearing loss. The otolaryngologist administered atranstympanic injection of a steroidfor the sudden hearing loss ineach ear. How is this reported?)
(Full Case:Established patient office visit.CC:Bilateral thyroid nodules.HPI:54-year-old evaluated for bilateral thyroid nodules; thyroid ultrasound last week showed multiple thyroid masses likely multinodular goiter; patient can “feel” left-sided nodules; denies dysphagia; denies unexplained weight loss/gain; family history thyroid cancer (maternal grandmother); otherwise no problems except palpable right-sided thyroid mass.ROS:Constitutional negative (chills/fever/weight change). ENT negative (hearing loss/trouble swallowing/voice change). GI negative (distention/pain/bleeding/bowel changes/N/V). Endocrine negative (cold/heat intolerance).PE:Vitals BP 140/72, P 96, R 16, T 97.6, SpO2 97%, wt 89.8 kg, ht 165.1 cm. General alert/cooperative/no distress. Head normocephalic. Throat moist/no lesions/no thrush. Neck: no adenopathy, supple, trachea midline,thyromegaly present, no carotid bruit, no JVD. Lungs clear. Heart regular rhythm/rate, normal S1/S2, no murmur/gallop/rub/click. Lymph nodes no palpable adenopathy.Assessment/Plan:Multinodular goiter; patient will have apercutaneous biopsy (minor procedure).Question:What E/M code is reported?)
An 8-year-old undergoes tonsillectomy with adenoidectomy for chronic tonsillitis and adenoiditis with hypertrophy.
What CPT® and ICD-10-CM codes are reported?
Which punctuation is used in the ICD-10-CM Alphabetic Index to identify manifestation codes?
A 60-year-old male has three-vessel disease and supraventricular tachycardia which has been refractory to other management. He previously had pacemaker placement and stenting of LAD coronary artery stenosis, which has failed to solve the problem. He will undergo CABG with autologous saphenous vein and an extensive modified MAZE procedure to treat the tachycardia.
He is brought to the cardiac OR and placed in the supine position on the OR table. He is prepped and draped, and adequate endotracheal anesthesia is assured. A median sternotomy incision is made and cardiopulmonary bypass is initiated. The endoscope is used to harvest an adequate length of saphenous vein from his left leg. This is uneventful and bleeding is easily controlled. The vein graft is prepared and cut to the appropriate lengths for anastomosis. Two bypasses are performed: one to the circumflex and another to the obtuse marginal. The left internal mammary is then freed up and it is anastomosed to the ramus, the first diagonal, and the LAD. An extensive maze procedure is then performed and the patient is weaned from bypass. At this point, the sternum is closed with wires and the skin is reapproximated with staples. The patient tolerated the procedure without difficulty and was taken to the PACU.
Choose the procedure codes for this surgery.
An 8-year-old patient is placed under general anesthesia for treatment of a right orbital fracture due to a traumatic fall to the nose and face from a swing set. An on-call otolaryngologist is
asked to perform a general otolaryngologic examination to evaluate the patient. A mild nasal fracture is the diagnosis given by the otolaryngologist.
What is the CPT® and ICD-10-CM coding for the otolaryngologist's services?
An interventional radiologist performs an abdominal paracentesis in his office utilizing ultrasonic imaging guidance to remove excess fluid. What CPT® coding is reported?
Refer to the supplemental information when answering this question:
View MR 874276
What E/M code is reported?
An elderly patient comes into the emergency department (ED) with shortness of breath. An ECG is performed The final diagnosis at discharge is impending myocardial infarction.
According to ICD-10-CM guidelines, how is this reported?
A patient arrived at the emergency department experiencing pain in both legs. The ED physician ordered a comprehensive duplex scan of the arteries in both lower extremities to rule out arteriosclerosis.
What CPT® and ICD-10-CM codes are reported?
(A patient is in her dermatologist’s office for treatment of recurring psoriatic plaques on the upper back and neck resistant to topical therapy. The dermatologist performsExcimer laser therapyon the upper back (300 sq cm) and neck (100 sq cm), total surface area400 sq cm. What CPT® codes are reported?)
A 25-year-old woman underwent percutaneous breast biopsy on the right breast with placement of a Gelmark clip. The procedure was performed using stereotactic imaging.
What CPT® codes will be reported?
(Full Case:Preoperative diagnosis:Recurrent dysphagia.Postoperative diagnosis:Hiatal hernia with obstruction.Procedure:EGD with dilation.Consent:PAR conference; informed consent signed; premedication given.Position/monitoring:left lateral decubitus; monitored with BP cuff and pulse oximeter throughout.Topical:Hurricaine spray to posterior pharynx.Scope passage:flexible endoscope passed under direct visualization through cricopharyngeus into esophagus; advanced with identification of EG junction into stomach; rugal folds visualized; advanced to antrum/pylorus; pylorus cannulated; duodenal bulb and second portion visualized; retroflexed views of cardia/fundus/lesser curvature.Dilation technique:guidewire placed in antrum; scope removed; wire positioned by markings;#14 French dilatorpassed into stomach area;esophageal dilation performed over guidewire.Findings:tortuous/shortened esophagus; large sliding hiatal hernia; EG junction ~30 cm; stomach abnormal with very large sliding hiatal hernia; duodenum normal.Question:What CPT® coding is reported?)
A physician excises a 3.5 cm malignant lesion including margins from the back. Then a destruction of a 2.0 cm benign lesion on the right cheek of the face with cryosurgery.
What CPT@ and ICD-10-CM is reported?
A complete 7-view X-ray of the lumbosacral spine, including bending views, is performed.
What CPT® code is reported?
Refer to the supplemental information when answering this question:
View MR 005271
What CPT® coding is reported?
A patient has five biopsies performed on the duodenum.
What CPT® coding is reported?
The CPT® code book provides full descriptions of medical procedures, with some descriptions requiring the use of a semicolon (;) to distinguish among closely related procedures.
What is the full description of CPT® code 35860?
A patient is diagnosed with sepsis and associated acute respiratory failure.
What ICD-10-CM code selection is reported?
A catheter was placed into the abdominal aorta via the right common femoral artery access. An abdominal aortography was performed. The right and left renal artery were adequately visualized. The catheter was used to selectively catheterize the right and left renal artery. Selective right and left renal angiography were then performed, demonstrating a widely patent right and left renal artery.
What CPT® coding is reported?
An otolaryngologist removes a 3 cm deep facial tumor within muscle.
What CPT® code is reported?
A 42-year-old with chronic left trochanteric bursitis is scheduled to receive an injection at the Pain Clinic. A 22-gauge spinal needle is introduced into the trochanteric bursa under ultrasonic guidance, and a total volume of 8 cc of normal saline and 40 mg of Kenalog was injected.
What CPT® code should be reported for the surgical procedure?
A patient is going to have placement of a myringotomy tube. This tube is placed in the ______ to drain excess fluid.
A patient undergoes CABG using the right internal mammary artery anastomosed to three coronary arteries.
What CPT® coding is reported?
A patient undergoes a laparoscopic appendectomy for chronic appendicitis.
What CPT® and diagnosis codes are reported?
What CPT® coding is reported for a subtotal thyroidectomy for malignancy with radical neck dissection?
A surgeon performed Mohs micrographic surgery on a lesion on the right arm. This required one stage with six tissue blocks.
What CPT@ codes are reported for the Mohs surgery?
A patient suffering from idiopathic dystonia is seen today and receives the following Botulinum injections: three muscle injections in both upper extremities and seven injections in six paraspinal muscles.
How are these injections reported according to the CPT® guidelines?
A 42-year-old male is diagnosed with a left renal mass. An abdominal incision along with rib resection is made to expose and access the kidney. The left kidney is removed, along with surrounding fat, adrenal gland, lymph nodes in the area, and the incision site is sutured. What CPT ® code is reported for this procedure?
(A 5-year-old patient has a fractured radius. The orthopedist providesmoderate sedationand the reduction. The intra-service sedation time is documented as21 minutes. What CPT® code is reported for the moderate sedation?)
A patient presents to the surgical suite for a planned sterilization procedure via a bilateral excisional vasectomy.
What is the correct CPT® code and diagnosis code for the service?
Which HCPCS Level II codes identify temporary services that would not be assigned a CPT® code, but are needed for claims processing purposes?
(A patient presents to the urgent care facility with multiple burns acquired while burning debris in his backyard. After examination the physician determines the patient hasthird-degree burns of the left and right posterior thighs (10%). He also hassecond-degree burnsof theanterior portion of the right side of his chest wall (8%)andupper back (6%).TBSA is 24%withthird-degree burns totaling 10%. What ICD-10-CM codes are reported, according to ICD-10-CM coding guidelines?)
A patient undergoes MRI-guided needle liver biopsy with two core samples taken.
What CPT® codes are reported?
(A patient presents with increased intracranial pressure and is scheduled for a lumbar puncture. UnderCT guidance, the physician inserts a needle at the L4 level and advances a catheter into the subarachnoid space toactively drain cerebrospinal fluid. CSF is collected and sent to the lab; the catheter is removed. What CPT® coding is reported?)
(The physician performs adiagnostic ERCPof the common bile duct with insertion of astentinto the biliary duct. What CPT® coding is reported?)
(A patient presents with dysuria and lower abdominal pain. The physician suspects UTI. Anautomated urinalysis without microscopyis done in the office and isnegative. UTI is ruled out for the final diagnosis. What CPT® and ICD-10-CM codes are reported?)
A patient has a 5 cm tumor in the left lower quadrant abdominal wall, excised through dermis and subcutaneous tissue. Pathology is pending to rule out cancer.
What CPT® and ICD-10-CM codes are reported?
(Day 1: Provider admits patient toobservation carefor type 2 diabetes with hyperglycemia, orders labs, consults endocrinologist, starts IV insulin drip, keeps overnight. Day 2: orders glucose test, dietitian, documents total time 25 minutes. Day 3: glucose normal, documents 15 minutes, discharges patient. What E/M coding is reported by the physician for the patient in observation care?)
A patient has suspicious lesions on his feet. Biopsies confirm squamous cell carcinoma. The patient elects to destroy a 0.6 cm lesion on the right dorsal foot and a 2.0 cm lesion on the left dorsal foot using cryosurgery.
What CPT® coding is reported?
A couple presents to the freestanding fertility clinic to start in vitro fertilization. Under radiologic guidance, an aspiration needle is inserted (by aid of a superimposed guiding-line) puncturing the ovary and preovulatory follicle and withdrawing fluid from the follicle containing the egg.
What is the correct CPT® code for this procedure?
A patient is diagnosed with a healing pressure ulcer on her left heel that is currently being treated.
What ICD-10-CM coding is reported?
A suppression study includes five glucose tests and five growth hormone tests.
What CPT® coding is reported?
What ICD-10-CM coding is reported for a patient who has hypertension and CKD stage 2?
(A 55-year-old female with severe coronary arteriosclerosis with angina is admitted for elective coronary artery bypass. The surgeon performed a coronary artery bypass using asaphenous vein harvested endoscopically. The vein graft was anastomosed to theobtuse marginaland theleft circumflex. What CPT® coding is reported for this procedure?)
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What E/M code is reported for this encounter?
A diagnostic mammogram is performed on the left and right breasts. Computer-aided detection is also used to further analyze the image for possible lesions.
What CPT® coding is reported for this radiology service?
Which circumstance supports medical necessity for a payment by the insurance company?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® coding is reported?
A 67-year-old patient has osteomyelitis of the shoulder blade and is in surgery to remove the sequestered section of dead infected fragment bone from surrounding bone.
What CPT® code is reported?
What is the medical term for a procedure that creates an opening between the bladder and the rectum?
A cystic lesion on the chest is excised with margins totaling 2.5 cm. Simple closure performed.
What CPT® coding is reported?
A surgeon performs midface LeFort I reconstruction on a patient’s facial bones to correct a congenital deformity. The reconstruction is performed in two pieces in moving the upper jawbone forward and repositioning the teeth of the maxilla of the mid face.
What CPT® code is reported?
A 43-year-old female with a history of joint pain and fatigue presents to the office with swollen salivary glands. Patient agrees to have a labial gland biopsy performed in office. Patient is
numbed with a local anesthetic. Then an incision is made on the lower labial mucosa and tissue samples from the salivary gland are removed with tweezers. The incision is sutured. Pathology
report findings are consistent with Sjogren's syndrome.
What CPT® code is reported?
A 6-French sheath and catheter is placed into the coronary artery and is advanced to the left side of the heart into the ventricle. Ventriculography is performed using power injection of contrast agent. Pressures in the left heart are obtained. The coronary arteries are also selected and imaged.
What CPT® code is reported?
A patient is having X-ray imaging of his abdomen following a traumatic episode. A decubitus, supine, and erect views are performed on the abdomen.
What CPT® is reported?
A patient suffers a ruptured infrarenal abdominal aortic aneurysm requiring emergent endovascular repair. An aorto-aortic tube endograft is positioned in the aorta and a balloon dilation is performed at the proximal and distal seal zones of the endograft. The balloon angioplasty is performed for endoleak treatment.
What CPT® code does the vascular surgeon use to report the procedure?
A patient with intermittent asthma with exacerbation undergoes spirometry before and after bronchodilator.
What CPT® and ICD-10-CM codes are reported?
56-year-old female is postmenopausal with abnormal vaginal bleeding. Ob-gyn provider performs a hysteroscopy to examine the uterine cavity.
What CPT® code is reported?
A patient comes in complaining of pain in the lower left back, which is accompanied by a numbing sensation that extends into the leg. Attempts to alleviate the pain with home treatments have been unsuccessful. The provider orders an MRI of the lumbar spine initially without, and then with, contrast material. The images are interpreted by the physician, the final diagnosis is left-sided low back pain with sciatica.
What CPT® and ICD-10-CM codes are reported?
A complete cardiac MRI for morphology and function without contrast, followed by contrast with four additional sequences and stress imaging, is performed on a patient with systolic left ventricular congestive heart failure and premature ventricular contractions.
What CPT® and ICD-10-CM codes are reported?
A 1-year-old patient has bilateral supernumerary digits:
Left digit contains bone and joint → amputated
Right digit is a soft-tissue nubbin → simple excision
What CPT® coding is reported?
View MR 005398
MR 005398
Operative Report
Preoperative Diagnosis: Nonfunctioning right kidney with ureteral stricture.
Postoperative Diagnosis: Nonfunctioning right kidney with ureteral stricture.
Procedure: Right nephrectomy with partial ureterectomy.
Findings and Procedure: Under satisfactory general anesthesia, the patient was placed in the right flank position. Right flank and abdomen were prepared and draped out of the sterile field. Skin incision was made between the 11th and 12th ribs laterally. The incision was carried down through the underlying subcutaneous tissues, muscles, and fascia. The right retroperitoneal space was entered. Using blunt and sharp dissection, the right kidney was freed circumferentially. The right artery, vein, and ureter were identified. The ureter was dissected downward where it is completely obstructed in its distal extent. The ureter was clipped and divided distally. The right renal artery was then isolated and divided between 0 silk suture ligatures. The right renal vein was also ligated with suture ligatures and 0 silk ties. The right kidney and ureter were then submitted for pathologic evaluation. The operative field was inspected, and there was no residual bleeding noted, and then it was carefully irrigated with sterile water. Wound closure was then undertaken using 0 Vicryl for the fascial layers, 0 Vicryl for the muscular layers, 2-0 chromic for subcutaneous tissue, and clips for the skin. A Penrose drain was brought out through the dependent aspect of the incision. The patient lost minimal blood and tolerated the procedure well.
What CPT® coding is reported for this case?
A 13-year-old established patient is seen for an annual preventive exam. Last visit was two years ago.
What CPT® code is reported?
View MR 007400
MR 007400
Radiology Report
Patient: J. Lowe Date of Service: 06/10/XX
Age: 45
MR#: 4589799
Account #: 3216770
Location: ABC Imaging Center
Study: Mammogram bilateral screening, all views, producing direct digital image
Reason: Screen
Bilateral digital mammography with computer-aided detection (CAD)
No previous mammograms are available for comparison.
Clinical history: The patient has a positive family history (mother and sister) of breast cancer.
Mammogram was read with the assistance of GE iCAD (computerized diagnostic) system.
Findings: No dominant speculated mass or suspicious area of clustered pleomorphic microcalcifications is apparent Skin and nipples are seen to be normal. The axilla are unremarkable.
What CPT® coding is reported for this case?
An established patient presents with fever and sore throat. Rapid strep test is positive.
What CPT® and ICD-10-CM codes are reported?
A 26-year-old male presents with a deep laceration from a kitchen knife to his right hand. The surgeon washes the open wound with sterile saline. Clamps are applied. The provider cleans the
vessel and prepares the edges of thee wound. She then repairs the bleeding vessel with sutures. The clamps are removed and the provider uses a Doppler probe to check the blood flow pattern
through the repaired vessel.
What CPT® code is reported?
An 87-year-old male with a history of atrioventricular block and prior dual-chamber pacemaker implantation presents to the cardiology clinic for an in-person device evaluation. The physician performs a full electronic analysis of the pacemaker system, assessing atrial and ventricular lead function, battery status, sensing thresholds, and pacing thresholds. After the assessment, the pacemaker settings are adjusted to optimize heart rate response. The patient tolerates the procedure well and is advised to return for routine follow-up.
What CPT® code is reported?
A 4-year-old, critically ill child is admitted to the PICU from the ED with respiratory failure due to an exacerbation of asthma not manageable in the ER. The PICU provider takes over the care of the patient and starts continuous bronchodilator therapy and pharmacologic support with cardiovascular monitoring and possible mechanical ventilation support.
What is the E/M code for this encounter?
(What CPT® coding is reported for the insertion ofHeyman capsulesfor clinical brachytherapy?)
(A 3-year-old is seen by his primary care physician for anannual exam. His last exam with the primary care physician wastwo years ago. He has no complaints. What CPT® code is reported?)
A comatose patient is seen in the ER. The patient has a history of depression. Drug testing confirm she overdosed on tricyclic antidepressant drugs doxepin, amoxapine, and clomipramine.
What CPT® code is reported?
(A 40-year-old woman with progressive sensorineural hearing loss in the right ear has acochlear implantplaced for the right ear. Anesthesia is provided by aCRNAwithmedical directionby an anesthesiologist who is concurrently directing 5 CRNAs. Physical status is3. What anesthesia CPT® and ICD-10-CM codes are reported by theanesthesiologist?)
A 19-year-old is seen by his, primary care physician for an annual exam. His last exam with the primary care physician was four years ago. He has no complaints.
What CPT code is reported?
Refer to the supplemental information when answering this question:
View MR 903096
What CPT® and ICD-10-CM coding is reported?
A 78-year-old patient experiencing intermittent asthma with exacerbation is in her pulmonologist's office for a pulmonary function test. The pulmonologist tests for spirometry, vital capacity,
breathing capacity, and flow volume capturing the measurements before and after administering a bronchodilator.
What CPT® and ICD-10-CM codes are reported?
A woman who is 19 weeks pregnant is taken to the hospital from her doctor's office due to the detection of no fetal heartbeat and the death of the fetus. Due to the stage of pregnancy, labor is initiated, and the fetus is delivered.
What CPT® and ICD-10-CM codes are reported for the delivery of the fetus on the maternal record?
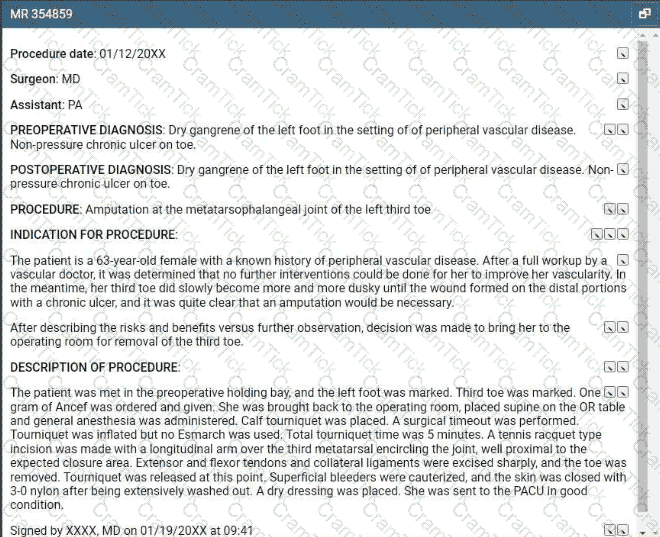
Refer to the supplemental information when answering this question:
View MR 354859
What CPT® and ICD-10-CM coding is reported?
Which government office is responsible for overseeing and investigating cases of healthcare fraud and abuse?
A patient with Parkinson's has sialorrhea. The physician administers an injection of atropine bilaterally into a total of four submandibular salivary glands.
What CPT® coding is reported?
The gynecologist performs a colposcopy of the cervix including biopsy and endocervical curettage.
What CPT® code is reported?
A wedge excision of soft tissue at the lateral margin of an ingrown toenail on the left great toe is performed.
What CPT® code is reported?
Mrs. Wilder presents with right and left leg swelling. Venous thrombosis imaging of each leg is done and shows deep venous embolism and thrombosis in each leg.
What CPT® and ICD-10-CM codes are reported?
A therapeutic colonoscopy is performed, where the scope goes beyond the splenic flexure, but not to the cecum. Using the Colonoscopy Decision Tree illustrated in the CPT® code book, what coding is reported?
The procedure is performed at an outpatient radiology department. From a left femoral access, the catheter is placed in the abdominal aorta and is then selectively placed in the celiac trunk and manipulated up into the common hepatic artery for an abdominal angiography. Dye is injected, and imaging is obtained. The provider performs the supervision and interpretation.
What CPT® codes are reported?
Which statement is TRUE for an Excludes2 note that is under a code in the Tabular List for ICD-10-CM?
During a laparoscopic hemicolectomy, the left kidney is accidentally perforated. A nephrologist performs open repair of the kidney laceration and places a JP drain.
What CPT® and ICD-10-CM coding is reported by the nephrologist?
View MR 001394
MR 001394
Operative Report
Procedure: Excision of 11 cm back lesion with rotation flap repair.
Preoperative Diagnosis: Basal cell carcinoma
Postoperative Diagnosis: Same
Anesthesia: 1% Xylocaine solution with epinephrine warmed and buffered and injected slowly through a 30-gauge needle for the patient's comfort.
Location: Back
Size of Excision: 11 cm
Estimated Blood Loss: Minimal
Complications: None
Specimen: Sent to the lab in saline for frozen section margin control.
Procedure: The patient was taken to our surgical suite, placed in a comfortable position, prepped and draped, and locally anesthetized in the usual sterile fashion. A #15 scalpel blade was used to excise the basal cell carcinoma plus a margin of normal skin in a circular fashion in the natural relaxed skin tension lines as much as possible The lesion was removed full thickness including epidermis, dermis, and partial thickness subcutaneous tissues. The wound was then spot electro desiccated for hemorrhage control. The specimen was sent to the lab on saline for frozen section.
Rotation flap repair of defect created by foil thickness frozen section excision of basal cell carcinoma of the back. We were able to devise a 12 sq cm flap and advance it using rotation flap closure technique. This will prevent infection, dehiscence, and help reconstruct the area to approximate the situation as it was prior to surgical excision diminishing the risk of significant pain and distortion of the anatomy in the area. This was advanced medially to close the defect with 5 0 Vicryl and 6-0 Prolene stitches.
What CPT® coding is reported for this case?
A cardiologist attempted to perform a percutaneous transluminal coronary angioplasty of a totally occluded blood vessel. The surgeon stopped the procedure because of an anatomical problem creating risk for the patient and preventing performance of the catheterization.
What modifier is appended to the procedure code?
Provider performs staged procedures for gender reassignment surgery converting female anatomy to male anatomy.
What CPT® code is reported?
View MR 003396
MR 003396
Operative Report
Preoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Postoperative Diagnosis: Acute MI, severe left main arteriosclerotic coronary artery disease
Procedure Performed: Placement of an intra-aortic balloon pump (IABP) right common femoral artery
Description of Procedure: Patient's right groin was prepped and draped in the usual sterile fashion. Right common femoral artery is found, and an incision is made over the artery exposing it. The artery is opened transversely, and the tip of the balloon catheter was placed in the right common femoral artery. The balloon pump had good waveform. The balloon pump catheter is secured to his skin after local anesthesia of 2 cc of 1% Xylocaine is used to numb the area. The balloon pump is secured with a 0-silk suture. The patient has sterile dressing placed. The patient tolerated the procedure. There were no complications.
What CPT® coding is reported for this case?
Patient is admitted in observation care on 12/2/20XX in the morning for acute asthma exacerbation. The ED physician requires the patient to stay overnight. Next day, 12/3/20XX the patient is
discharged from observation care in the afternoon. Patient's total stay in observation was 16 hours.
What E/M categories and code ranges are appropriate to report?
A patient has chronic cholesteatoma in the right middle ear. The otolaryngologist performed a tympanoplasty with a radical mastoidectomy, removing the middle ear cholesteatoma. Grafting
technique was used to repair the eardrum with ossicular chain reconstruction.
What CPT® code is reported for this surgery?
A patient with severe diverticulitis in the sigmoid colon presents to surgery for a partial colectomy. The physician performs an exploratory laparoscopic laparotomy to verify the location of the diverticulitis. Once identified, it was noted that there was bleeding from the diverticulitis. The physician transects the descending colon and then transects at the line of the rectum.
The physician mobilizes the splenic flexure in order to create a colostomy with the proximal portion of the remaining colon. The distal portion of the colon is closed. The physician washes the patient's abdomen with saline, removes all trocars and instruments, and then closes the abdomen with sutures.
What CPT® and ICD-10-CM codes are reported?
A 52-year-old male patient with known AIDS saw his orthopedic physician today for severe pain in the right knee. The physician documents that his knee pain is due to a flare up of posttraumatic osteoarthritis and he gives him a cortisone injection in the right knee joint. The osteoarthritis is not related to AIDS.
What ICD-10-CM codes are reported for this encounter?
A woman at 36-weeks gestation goes into labor with twins. Fetus 1 is an oblique position, and the decision is made to perform a cesarean section to deliver the twins. The obstetrician who delivered the twins, provided the antepartum care, and will provide the postpartum care.
What CPT® coding is reported for the twin delivery?
What is the medical term for a procedure that creates a connection between the gallbladder and the small intestine?
The CPT® code book provides full descriptions of medical procedures, although some descriptions require the use of a semicolon (;) to distinguish among closely related procedures.
What is the full description of CPT® code 69644?
A patient undergoes a percutaneous liver biopsy with ultrasound guidance for primary biliary cirrhosis.
What CPT® and ICD-10-CM codes are reported?
A 3-day-old died in her sleep. The pediatrician determined this was the result of crib death syndrome. The parents give permission to refer the newborn for a necropsy. The pathologist receives the newborn with her brain and performs a gross and microscopic examination. The physician issues the findings and reports they are consistent with a normal female newborn.
What CPT® code is reported?
A Medicare patient is scheduled for a screening colonoscopy.
What code is reported for Medicare?
A patient with malignant lymphoma is administered the antineoplastic drug Rituximab 800 mg and then 100 mg of Benadryl.
Which HCPCS Level II codes are reported for both drugs administered intravenously?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
Which CPT® and ICD-10-CM codes are reported for this procedure?
A pediatrician removes impacted cerumen using irrigation in the right ear and instrumentation in the left ear.
What CPT® coding is reported?
The provider orders a bile test for a patient that has chronic hepatitis that is undergoing treatment. Lab analyst quantitates the total bile acids with an enzymatic method. What CPT® code is
reported for the test?
View MR 002395
MR 002395
Operative Report
Pre-operative Diagnosis: Acute rotator cuff tear
Post-operative Diagnosis: Acute rotator cuff tear, synovitis
Procedures:
1) Rotator cuff repair
2) Biceps Tenodesis
3) Claviculectomy
4) Coracoacromial ligament release
Indication: Rotator cuff injury of a 32-year-old male, sustained while playing soccer.
Findings: Complete tear of the right rotator cuff, synovitis, impingement.
Procedure: The patient was prepared for surgery and placed in left lateral decubitus position. Standard posterior arthroscopy portals were made followed by an anterior-superior portal. Diagnostic arthroscopy was performed. Significant synovitis was carefully debrided. There was a full-thickness upper 3rd subscapularis tear, which was repaired. The lesser tuberosity was debrided back to bleeding healthy bone and a Mitek 4.5 mm helix anchor was placed in the lesser tuberosity. Sutures were passed through the subcapulans in a combination of horizontal mattress and simple interrupted fashion and then tied. There was a partial-thickness tearing of the long head of the biceps. The biceps were released and then anchored in the intertubercular groove with a screw. There was a large anterior acromial spur with subacromial impingement. A CA ligament was released and acromioplasty was performed. Attention was then directed to the
supraspinatus tendon tear. The tear was V-shaped and measured approximately 2.5 cm from anterior to posterior. Two Smith & Nephew PEEK anchors were used for the medial row utilizing Healicoil anchors. Side-to-side stitches were placed. One set of suture tape from each of the medial anchors was then placed through a laterally placed Mitek helix PEEK knotless anchor which was fully inserted after tensioning the tapes. A solid repair was obtained. Next there were severe degenerative changes at the AC joint of approximately 8 to 10 mm. The distal clavicle was resected taking care to preserve the superior AC joint capsule. The shoulder was thoroughly lavaged. The instruments were removed and the incisions were closed in routine fashion. Sterile dressing was applied. The patient was transferred to recovery in stable condition.
What CPT® coding is reported for this case?
View MR 099405
MR 099405
CC: Shortness of breath
HPI: 16-year-old female comes into the ED for shortness of breath for the last two days. She is an asthmatic.
Current medications being used to treat symptoms is Advair, which is not working and breathing is getting worse. Does not feel that Advair has been helping. Patient tried Albuterol for persistent coughing, is not helping. Coughing 10-15 minutes at a time. Patient has used the Albuterol 3x in the last 16 hrs. ED physician admits her to observation status.
ROS: No fever, no headache. No purulent discharge from the eyes. No earache. No nasal discharge or sore throat. No swollen glands in the neck. No palpitations. Dyspnea and cough. Some chest pain. No nausea or vomiting. No abdominal pain, diarrhea, or constipation.
PMH: Asthma
SH: Lives with both parents.
FH: Family hx of asthma, paternal side
ALLERGIES: PCN-200 CAPS. Allergies have been reviewed with child’s family and no changes reported.
PE: General appearance: normal, alert. Talks in sentences. Pink lips and cheeks. Oriented. Well developed. Well nourished. Well hydrated.
Eyes: normal. External eye: no hyperemia of the conjunctiva. No discharge from the conjunctiva
Ears: general/bilateral. TM: normal. Nose: rhinorrhea. Pharynx/Oropharynx: normal. Neck: normal.
Lymph nodes: normal.
Lungs: before Albuterol neb, mode air entry b/l. No rales, rhonchi or wheezes. After Albuterol neb. improvement of air entry b/l. Respiratory movements were normal. No intercostals inspiratory retraction was observed.
Cardiovascular system: normal. Heart rate and rhythm normal. Heart sounds normal. No murmurs were heard.
GI: abdomen normal with no tenderness or masses. Normal bowel sounds. No hepatosplenomegaly
Skin: normal warm and dry. Pink well perfused
Musculoskeletal system patient indicates lower to mid back pain when she lies down on her back and when she rolls over. No CVA tenderness.
Assessment: Asthma, acute exacerbation
Plan: Will keep her in observation overnight. Will administer oral steroids and breathing treatment. CXR ordered and to be taken in the morning.
What E/M code is reported?
(A provider documents “pericarditis with effusion” in the assessment. Based on medical terminology, which structure is inflamed?)
Which one of the following is correct to report an intermediate repair code (12031–12037)?
A patient with jaundice was seen by the physician to obtain liver biopsies. A needle biopsy was taken using CT guidance for needle placement. The physician obtained two core biopsies, which
were then sent to pathology. What CPT® codes are reported?
A patient is brought to the operating room with a right-sided peripheral vertigo. The provider makes a postauricular incision and uses an operating microscope to perform a mastoidectomy using a burr. He next destroys the semicircular canals, the utricle, and saccule completely removing the diseased labyrinth structures. The provider sutures the incision.
What CPT® code and ICD-10-CM codes are reported?
An established patient suffering from migraines without aura, no mention of intractable migraine, and no mention of status migrainosus, is seen by his ophthalmologist who conducts a visual field examination of both eyes. The examination was accomplished plotting four isopters utilizing the Goldmann perimeter testing method. The patient and requesting physician receive the interpretation and report on the same date of service.
What procedure and diagnosis codes are reported for this encounter?
A provider performs a mastoidectomy and complete labyrinthectomy for right-sided peripheral vertigo.
What CPT® and ICD-10-CM codes are reported?
A patient presents to the pulmonologist's office for the first time with coughing and shortness of breath. The patient has a history of asthma. The physician performs a medically appropriate
history and exam. The following labs are ordered: CBC, arterial blood gas, and sputum culture. The pulmonologist assesses the patient with a new diagnosis of COPD. The patient is given a
prescription for the inhaler Breo Ellipta.
What E/M code is reported?
(A physician performsexcisional debridementfor a patient with multiple wounds. A wound on thelower backmeasures12 cmand involves thefasciafor the debridement. A wound on theleft shouldermeasures8 cmand one on theleft lower legmeasures16 cminvolvessubcutaneous tissuefor the debridement. What CPT® codes are reported?)